What is Frozen Shoulder?
Frozen Shoulder is when the capsule that surrounds the shoulder joint gradually tightens and causes pain and restricted movement of the shoulder. This often leads to pain and disability.
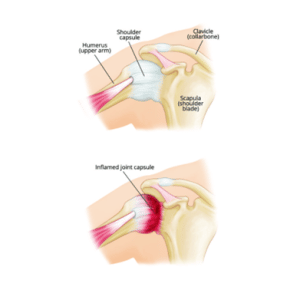
Frozen Shoulder is when the capsule that surrounds the shoulder joint gradually tightens and causes pain and restricted movement of the shoulder. This often leads to pain and disability.
We do not fully know what causes this condition. Sometimes a specific event will happen, such as a fall or bump, although most of the time there is no obvious cause.
Frozen shoulder is quite common in people aged 40-60, is more common in women, and is more common in people who have diabetes, cardiovascular disease, high cholesterol or thyroid disease.
About 10% of people can expect to experience the same symptoms in their other shoulder in the future. This risk is higher in people with diabetes.
People often experience significant pain and very restricted movements, twisting your arm may be the most problematic. The pain can last for between two and nine months and unfortunately, it can take anywhere between a year and four years to fully resolve.
The shoulder joint capsule thickens over time which limits movement of the shoulder. When the symptoms start to improve it tends to be a slow process. Your shoulder may always have some restriction of movement in the future. Although the pain usually gets better, it may never go away completely.
Symptoms may include:
• Pain in the shoulder and upper arm
• Pain can be severe in the early days and may be constant, which can interfere with your sleep.
• Pain can be a lot worse on reaching for things or when lying on the affected side.
• Some people notice that as the pain settles the stiffness gets worse
• The shoulder may then stiffen up quickly. – how much it stiffens is very variable
• The restricted movement can stop you from putting your hand behind you, or being able to reach as far as the back of your head.
No one treatment has been shown to ‘cure’ a frozen shoulder and on average a frozen shoulder can last about two and a half years.
The aims of treatment are:
Most treatment options are about pain control, accepting the limitations of the shoulder and waiting for it to get better.
Over the counter painkillers like paracetamol or ibuprofen will ease the pain, but need to be taken regularly in order to control the pain. Follow the instructions on the packet and discuss using them safely with a pharmacist or GP, especially if you have any underlying health conditions.
Using a heat or cool pack on a painful shoulder might help to relieve the pain
Both heat and cool can be helpful but be careful not to put ice or heat packs or hot water bottles directly on your skin – wrap them with a tea towel or cover.
It important to remember that shoulders are designed to move, and inactivity can cause further problems with the tissues around the joint. With a frozen shoulder pain does not equal damage. It is therefore important to maintain movement within the limits of your pain.
However, you may want to avoid doing tasks that aggravate your pain too often. Adjusting how you do certain tasks can help manage your pain, for example, putting your sore arm in first to a jumper or jacket and taking it out last.
The British Elbow & Shoulder Society have created a video with useful exercises and information about frozen shoulder.
The British Elbow & Shoulder Society Frozen Shoulder exercise videoIf your symptoms aren’t improving after trying this advice for a couple of months or your pain is severely impacting on your ability to function, you should seek support from a healthcare professional. They may recommend referral onto a physiotherapist or other treatment.