Persistent or ‘chronic’ pain is a term that is often used by medical professionals to describe pain that persists for several months or even years.
It is often not clear why back pain becomes a persistent problem.
Even if a structural cause can be found, such as disc or facet joint degeneration, or muscle or ligament strain, pain may continue after the original problem has settled.
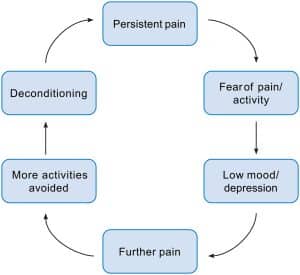
When you are experiencing pain, your natural reaction may be to avoid normal movements and activities.
However, this can lead to muscles becoming weaker and joints becoming stiffer, which can make you more susceptible to further problems. This is commonly known as deconditioning.
The neural pathways and pain receptors within the brain can also become used to experiencing pain, which can lead them to be more sensitive to stimulation that otherwise would not cause pain.
A person’s mood and emotional wellbeing can also impact upon the severity and duration of pain. For example, your pain may be more severe during or following a particularly stressful time.
Living with chronic pain can affect many aspects of your life, such as work, social activities and relationships. It can have an effect on how you live your life, as you may start avoiding doing the things that you enjoy doing.
However, this can lead to further deconditioning, making the chronic pain cycle worse.
It is important to try and stay as active as you can when the pain first begins. This will avoid deconditioning and pain becoming persistent.
Recovery – the good news!
For the majority of people, the chance of recovery from back pain is good, with 75 to 90 per cent recovering within weeks.
Back pain can return, especially as we get older, but this can be managed each time effectively by following the advice given on this page.