Exercise
Strengthening your thigh and hip muscles is helpful in controlling your whole lower limb movement and may help to prevent irritating the fat pad in day to day activities.
A rough guide would be to perform 8-12 repetitions of each exercise and 2-4 sets of these repetitions. Allowing a break of 30 seconds to 1 minute between sets is advisable. Pain can help guide numbers of repetitions and sets. Exercises should be carried out every other day.
Inner range quadriceps
Stand with leg slightly bent and exercise band above knee, attaching band to table leg or similar.
Tense muscles in the front of your thigh, straightening your knee and pulling back against the band.
Slowly release the band so your knee bends again.

Wall Squat
Stand with your knees bent at 45 degrees, leaning your back against the wall. Your feet should be at least 30cm away from the wall and hip width apart; make sure you can see your toes.
Keep your thigh muscles tightened the whole time. Aim to hold this position for 10 seconds. Feel in the front of your thigh. If this increases your pain, try with your feet further apart.

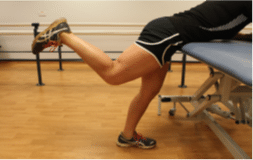
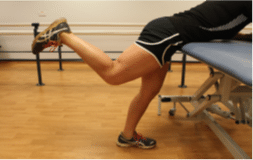
Standing leg lifts
Stand facing a worktop with your feet slightly wider than your hips. Lean forwards and rest on your forearms. Bend your knee. Lift your foot to the ceiling using your bottom muscles.